Events | IBD
On January 30, 2021, I was lucky enough to have the time to attend the Crohn’s and Colitis Foundation’s “IBD Insider: Patient Updates from the Crohn’s and Colitis Congress.” IBD Patient Insider is an education program for patients and their families, which summarizes information from the latest research presented annually at the Crohn’s and Colitis Foundation and the American Gastroenterological Association’s multi-disciplinary conference’s Crohn’s and Colitis Congress. As someone who spends a great deal of time in scholarly databases mining for the latest research, I was excited to learn from the speakers and get a glimpse at the future of IBD care. I was even more excited to then be able to share this with my community here at Girls with Guts. Unfortunately, despite the webinar providing fantastic information that will positively impact us, it was not as simple as attending and reporting back.
When Remicade was first being used to treat IBD, my pediatric Gastroenterologist was thrilled. She believed that with the breakthroughs that led to a biological treatment that a cure was right around the corner. Twenty-three years after Remicade was approved for IBD patients, I began the 2021 IBD Patient Insider webinar excited to learn about advances. Unfortunately, my excitement for IBD Insider waned not even three minutes into the seminar when the opening speaker, Dr. David T Rubin, ended his introduction to the webinar with, “I want one of the main takeaway messages for all of you to be today that: You can control your disease. You can ask the right questions. You should be empowered to understand how to live a better life despite a diagnosis of Crohn’s Disease or Ulcerative Colitis.”
For this IBD patient, Dr. Rubin’s emphasis on controlling IBD flew in the face of everything I have learned in 28 years with Crohn’s Disease (CD). For me, CD has always meant I cannot control what happens related to my IBD, but I can control how I react to it. The times I have foolishly thought I had control have all led me to the deepest darkest depressions in my life. The times I have dared to give in to the illusion that I can control IBD have led me to personalize medication failure or the emergence of a new symptom or extraintestinal manifestation. As I reflected on Dr. Rubin’s opening words in the context of the entire seminar, I think what Dr. Rubin meant was that with the advancements in understanding IBD, more patients have access to treatments that can help them better control and manage their IBD. But these words matter.
Words mattered to me when my pediatric GI’s optimism over Remicade fell short. As one of the earlier IBD patients on this medication before the advancements that led to biological medication drug level monitoring and antibody surveillance, I was one of those who, after months of treatment, ended up with an anaphylactic reaction and had to return to older treatment methods. “If this is the future,” I thought, “then I guess the cure won’t be for me.” However, even though my pediatric GI was a bit overoptimistic about Remicade, she was my doctor for fifteen years, and I was blessed that, in general, she was far ahead of the GI community in her approaches to care. Like my pediatric GI’s misstep with words, I am sure that Dr. Rubin was so excited to offer us patients a glimpse into a world where we suffer less his optimism bled through into his introduction. Even more, Dr. Rubin’s word began to fade as I became quickly hopeful about the research presenting during one of my favorite parts of IBD Insider, Dr. Brigid Boland’s presentation on “Future Therapies in IBD.”
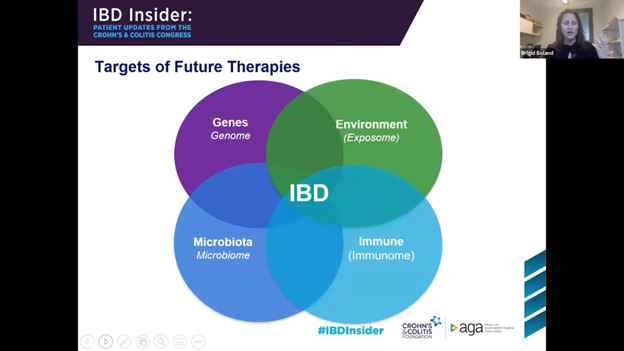
Dr. Boland’s presentation hit on the realities of IBD care as we currently know it as she openly expressed, “what we currently have is not quite what we want.” However, she explained that new therapies and approaches are being developed to address the current treatment gaps. For example, she explained that new therapies would address solutions for those with refractory IBD that currently respond to nothing, be more targeted with fewer side effects, and increase convenience with using small molecules to create pills instead of shots and infusions. Even more new research is revealing other treatments that address more than just the immune system. For instance, Boland explained that targets of future therapies would include genes, microbiota, and the environment. While the major presentations did an excellent job balancing the reasons for hope with the realities, throughout Insider as I listened and took notes, I continued to struggle with the way the program opened.
Today, at Insider, personalized medicine, holistic approaches to care, and getting the most out of your medical appointments were all parts of the presentations. Yet, as I can’t help but reflect and think back to years ago, it was my pediatric IBD GI, who first had me try holistic and complementary therapies like probiotics and specific diets. Furthermore, it was she who encouraged my tracking of symptoms, diet, and medication side effects. Long before patient satisfaction was tied to reimbursement and the emphasis on patient-centered care, my pediatric GI taught me to bring a notebook to appointments and write down my questions in-between appointments. Even more impressive for a pediatric physician it was Dr. Susan Edwards who was the first doctor I had ever known to offer me a place at the center of my care team, and for that I will always remain grateful.
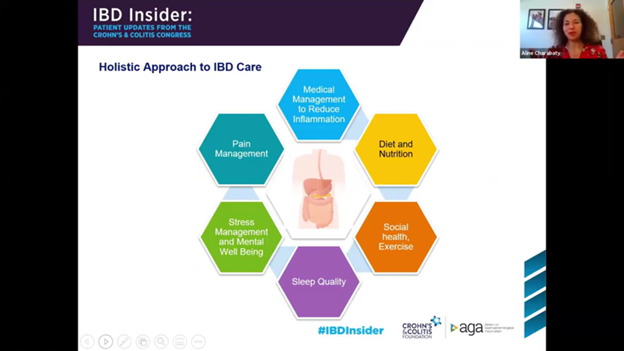
These IBD survival skills of being my own advocate and being the chief expert on me were reinforced with Dr. Rajeev Jain’s part of Insider on “Getting the Most out of Your Healthcare Visit.” Dr. Jain emphasized those same skills, Dr. Edwards taught me years ago. Furthermore, it was encouraging during Dr. Aline Charabaty’s presentation on “Holistic Approach to IBD Care” to see that the current research is diving deep into understanding IBD in the context of the whole person. It was energizing to learn more about specific diet therapies, obtain a better understanding of the relationships between stress and IBD flare, and even seeing investigations into the connections within shared decision-making and patient well-being.
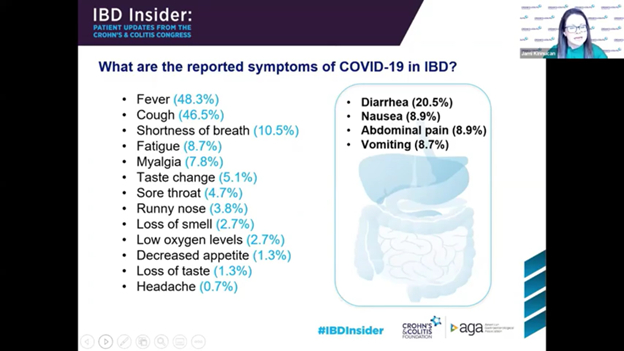
Naturally, IBD Insider also included the latest information from the research about COVD-19 and IBD. Luckily, the research has revealed that COVID-19 does not present an increased risk for most IBD patients. However, for those older in age (60 or older), who have multiple conditions with active disease and/or are on steroid treatments, the risk is higher. Furthermore, the medication used to treat IBD plays a role in the risk level related to COVID-19. There may be a possible increased risk for patients on mesalamine, and for those on combined Ant-TNF treatments, Thiopurine monotherapy (i.e., 6MP, etc.), or corticosteroids, there are increased risks. Ultimately, avoiding IBD flare is one of the most critical protective factors to minimize COVID-19 risk. To that end, IBD patients need to continue seeing their providers and treating their disease. With the recent COVID-19 Vaccinations, IBD patients were not included in the trials. However, the research community has determined that there are no safety concerns with the vaccines at this time. These conclusions are made from other data and previous vaccination. The only question remains how effective the vaccine will be for IBD patients, especially those on corticosteroids. Even though there may be decreased vaccine effectiveness in the IBD population, given the potential risks of COVID-19, even decreased effectiveness is still more protection than no vaccination.
Due to Dr. Rubins’ statements’ relatively short nature compared to all the positive parts of IBD Insider, I hesitated to include my reactions to Dr. Rubin’s words in this blog. I did not want to include such an emotionally charged part of IBD in this blog simply meant to celebrate how far the IBD community has come with an overview of this latest research. However, as I spent the week writing draft after draft, I could not help but wonder how I can be a trustworthy voice if I ignore the glaring overoptimistic introduction that hits every part of my IBD journey’s emotional aspects. Even more, these words almost prevented me from hearing the fantastic news that the IBD research community was presenting us with, and that news was incredibly positive and encouraging.
Except for those emotionally charged few moments at the beginning of the webinar, I was excited and energized around the many reasons for hope within each of the major presentations. Those reasons for hope offered by the research community give us a glimpse into a more personalized, targeted, and holistic approach to IBD care. Furthermore, shifts in American values related to healthcare have changed the cultural view that doctors are Gods who have the only voices that matter to a reality where doctors and patients are finally viewed as collaborators in the care team. For this IBD patient, the overall takeaways from IBD Insider were hope for the future with an increased awareness of the power of words and the need to consider how we all frame optimism and reality carefully. If you are interested in learning more or watching a recording of the entire ninety-minute presentation, you can find it here https://www.crohnscolitisfoundation.org/ibdinsider
