Coping | IBD
That’s how long it’s been since I’ve allowed myself to write. So I’m hoping what’s about to follow is coherent; in the event that it’s not… well, this was my disclaimer of responsibility.
Last week I was on the set of a video shoot for Janssen Biotech, Inc., the company that manufactures Remicade, to talk about my experience on the biologic, and how adding it to my treatment plan six years ago has since changed my life.
I was caught up in the conversational interview, and I’d warmed up enough to feel comfortable. I was telling my story, and most of that came naturally. But when the director posed this question about depression, I paused.
Suddenly my surroundings felt overly apparent. I noticed the camera lenses pointed at me from every angle, the sea of cables strewn across the floor. I felt the heat of the spotlights, the eyes of 40+ people on me, waiting for me to say something. And sitting in my tiny chair in the middle of all this felt like balancing on a pinhead.
It’s not that I had to think about the answer—it’s that I knew I was about to say something I could never take back. I’ve written a little about the correlation between mental health and chronic illness (and how it’s affected me), but typing words from behind a screen is one thing; looking directly into a camera and publicly disclosing potential hiccups in your mental health is another. Why? Because we all know the stigma associated with depression and anxiety. I thought, if people have told me to ease my IBD symptoms by putting mind over matter, I can only imagine the response this kind of sharing might prompt.
So I paused. But only for the few seconds it took me to decide I didn’t care about that kind of judgment anymore.
Of course I did. So that’s what I said when I looked at the director, and into the camera.
I was sick for months with no explanation of what was happening to my body. I was a college freshman trying to keep up academically and socially, while spending hours in the bathroom doubled over in pain. I was 18 years old and weighed 86 pounds, thought I was dying, constantly listened to those closest to me explain my symptoms away as stress. And my validation, my “relief,” was being told I have a chronic, incurable illness. I lived in pain for the better part of three years, while trying to lead a normal life as a young adult. I missed out on fun events and trips, habitually canceled plans with friends, ruined countless birthdays and holidays. I rode in the ambulance when my mom had a stroke in the aftermath of my diagnosis. I felt extremely isolated, confused, defeated, angry and lost—and then embarrassed for feeling all that.
I admitted all this on camera because I decided it would be riskier not to share the darker parts of my story than it would be to open myself up to scrutiny. Because the reason I was sitting there in the first place was to help people realize they’re not alone in their struggles, and that things can get better. In order to do that, I had to be honest, and that meant telling the whole story—not just the fragments I’m comfortable talking about and used to recounting.
I admitted all this on camera because a significant part of me felt alone for the first four years after my diagnosis, until I met other people living with IBD—people who finished my sentences, and not only told me it was okay to feel the way I did, but made me believe it was okay. I only wish someone had whispered that in my ear four years earlier.
After my mom had her stroke, I felt a strong sense of guilt. And then every hospital admission, every canceled plan, every holiday spent in bed only compounded that guilt, not to mention the fear of missing out. I remember lying in my hospital room at one point thinking I had some obscure illness that couldn’t be fixed and that, if I was this much of a burden at 20, I’d only be more so at 30, 40, and so on. I asked myself, Who would want to put up with that? And is it fair to ask that of anyone? What I’ve never shared before is a thought that crept up every now and then when I was sickest—that the people closest to me would be better off without the frustration, the unpredictability, the medical bills, the way everything in my life (at least, at the time) seemed to revolve around this relentless disease.
I didn’t talk about a lot of this back then because I didn’t think anyone would understand. If only I could travel back in time and bring along the network of support I have today. It wouldn’t have magically solved my problems, but talking to people who’d walked in my shoes would’ve saved me a lot of racing thoughts, and certainly would’ve provided me with better coping mechanisms.
Finding the right treatment plan and the right support system made a world of difference for me, as did giving back to the community and feeling like I was “doing my part” to fight this thing that had been taking control. But as there’s currently no cure for Crohn’s disease, there’s also no magic wand to disappear those feelings for good.
Yes, I did. More than I’d like to admit. And more recently that I’d like to admit.
When people tell you that you’re strong, that you’re an inspiration, that you’re a fighter, that you have such a positive outlook, you don’t want to stop them and admit you’re none of those things, and that you don’t really have a choice in the matter. That you still get overwhelmed, still spend days in bed, still have moments when it hits you all over again that you’re chronically ill, which means you’re most likely never going to feel 100%. That you can learn to deal with lesser symptoms when the major pain dies down, but that doesn’t mean you’ll ever be okay with them. You don’t want to show weakness or tear yourself down when someone else is building you up.
But you know what I’ve learned? I’ve learned that it takes more courage to admit those things than it does to keep them bottled up. That no one is okay all the time, and that people respect you more for sharing your struggles than pretending you don’t have them. I’ve learned that most people want to listen, want to help. And those who may not aren’t people worth worrying about.
So here I am admitting that I have some work to do. Here I am admitting that yes, I’ve used my health as an excuse to close myself off and push people away. Here I am admitting that recently, I’ve felt like I’m drowning, like I’m stuck. And like I haven’t been able to give as much of myself as I should to my career, to my friendships and other relationships, to my various commitments. And maybe I’ll post something that comes off confident and optimistic. Or maybe I’ll give you advice you find helpful. And maybe that leads you to think I don’t struggle with myself, that it’s just you. But that’s far from true; some things are just harder to share.
Mental health and physical health are more alike than we realize, and the same goes for depression and anxiety in comparison to chronic and invisible illnesses like IBD—they’re different for everyone, and they present in different ways, at different strengths, over different times.
Your feelings, your worries, your pain, your anxieties, they’re all valid. It’s okay to have them, and it’s more than okay to talk about them. They’re part of your story, and many more stories than you realize, waiting to be told by people who aren’t sure whether to share.
So when you’re faced with an important question you’re not sure if you should answer, like I was, try giving an honest response. In order to create a dialogue, someone has to speak first.
Yes, sometimes I did. Sometimes I still do. But I’m working on it. I’m talking about it. It took me seven months to write about this stuff again, but I did it. All because I answered a very private question in a very public way and, after hearing the support from everyone one room over in the studio, I had no desire to take it back.
So now you know.
How about you?
If you need to reach out to anyone, please don’t hesitate to use these resources:
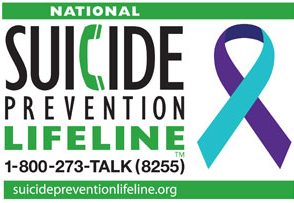
National Suicide Prevention Lifeline – 1-800-273-TALK (1-800-273-8255)
Crisis Text Line – Text “TWLOHA” to 741-741
[Both resources are available 24×7]

“I admitted all this on camera because I decided it would be riskier not to share the darker parts of my story than it would be to open myself up to scrutiny. Because the reason I was sitting there in the first place was to help people realize they’re not alone in their struggles, and that things can get better. In order to do that, I had to be honest, and that meant telling the whole story—not just the fragments I’m comfortable talking about and used to recounting.” THIS. Keri, thank you so much for sharing the whole story…not just the fragments or pieces. I am convinced that there can never be too many reminders that one is not alone. Your advocacy is making a huge difference!
Thank you for this! I so needed to hear it.
I’m not a girl but I do/did have Crohn’s disease. Suffered daily for six months before wishing the pain would kill me as I laid on my bed roing around and holding my stomach. After I hit a year of suffering, I nearly died from deep vein thrombosis and a pulmonary embolism that all my doctors said was caused by my Crohn’s. I remember being in the ER and wishing I had stayed out one more day because the doctor told me if I had then I wouldn’t have made it. Fast forward another 8 months, of taking 20+ pills a day, doing weekly injections, and continuously losing weight, I was finally told my colon had to be removed. At the time I thought that I could deal with the aftermath, and that it would significantly improve my life. That was six months ago, and I’m fighting depression now worse than my most pained days, and I don’t know why. I have no energy and I can’t explain it to my family anymore because they don’t understand. But I am going to go see a psychiatrist to try and get help. And I just randomly stumbled upon this blog tonight while I’ve been unable to sleep (because I’m still dealing with withdrawals from pain meds that I pretty much got addicted to). Thank you for showing that we’re not alone. All I’ve been needing is for someone to say that it’s okay to not be okay. I don’t know when I’ll be okay and I don’t know when I’ll be myself again. But I know I’m not alone.
Thanks for writing, Josh. You’re definitely not alone and even though the tunnel is long and dark, it does have an end. It ALWAYS has an end and there will be light. Just remember that the universe doesn’t work on your timeline, which means even when you think you’ve had enough it may not be time for things to change. But they will always change. Hang in there.
I have known I’ve had Crohn’s or ibd problem since I was about 21 finally after unable to control it by food and fasting finally collapsed 3 months after going to the doctors and waiting for referral to specialist so instead went in ambulance and spent a week in hospital then finally diagnosed nearly 2 years ago! Since then tried every medication ! Now manifested into joint pains and skin problems! On last infusion treatment now ! At one point when had reaction to treatment was stopped and was on no treatment or medication for a week then ended up bed bound couldn’t even move out of bed without help was horrible and happened so quick