Coping | IBD

Ten years. That’s how long it took to be diagnosed with Crohn’s Disease. I remember that first doctor’s visit vividly. I was home from my first year of undergrad and looking forward to lounging around and enjoying the summer with my family. But after almost every meal, I started having terrible abdominal pain and diarrhea.
I mentioned it to my mother who suggested I write down the things I’d eaten right before a stomach upset to try to determine the cause. I did. My symptoms continued, especially whenever I ate fruit and vegetables.
Sometimes, though, it would hurt when I hadn’t eaten anything at all. It was time to see a doctor, and I prepared to be told that I had some sort of food allergy. I hardly got through my complaint before he said, “Eat more fruit.” Huh? That’s like telling someone who tripped in broken high heels to keep wearing them. So I took his advice with a grain of salt. I was more careful around fruit and eliminated the ones that seemed to cause the most trouble.
Then I started having the same symptoms with other foods. With coffee, with pasta, oatmeal, yogurt, and bagels. Weren’t some of these foods supposed to be good for me? Why was I running to the bathroom in pain almost immediately after eating things that were healthy?
I went to another doctor. This one was worse. She grilled me about stress in my life. “Tell me about your boyfriend.” I didn’t have a boyfriend. “Are you sure?” Uh, yeah, I’m sure there’s no boyfriend. That was the end of the appointment and my faith in her. More time went by, more foods added to the list to avoid. Good-bye to popcorn, salads, strawberries, and sandwiches.
I went back to school. My symptoms subsided, and I started reincorporating foods back into my diet. There would be a day every now and then when I had to run to the bathroom, instantly berating myself for not keeping track of what I’d eaten. Maybe it was the mashed potatoes I’d eaten with dinner. Or the Caesar salad I’d had the day before.
There seemed to be no rhyme or reason to my symptoms and, because they’d become occasional, I didn’t dwell on the issue. By the time summer rolled around again, I felt confident. Last summer must have been a fluke, I was feeling much better these days. And then, almost in the blink of an eye, all my symptoms returned. Every food seemed to be a trigger and I couldn’t figure it out.
I went to a third doctor. She told me my symptoms sounded like Irritable Bowel Syndrome (IBS). I wore that label for a while, researched foods to avoid, and tried different ways to decrease stress, which I learned could also contribute to symptoms flaring up. I continued like this for a few more years, tip-toeing around my personal digestive troubles, chalking it all up to “tummy troubles” that I didn’t dare to explain to my friends.
In the fall of 2012 I started graduate school. That summer had been especially rough, and I’d lost around 15 pounds from avoiding many foods, and immediately going to the bathroom when I did eat. I figured that things would be better when my classes started and I could establish some routine. I was wrong. Between August and October that year, I lost another 20 pounds. I had resorted to eating only white rice and sipping on peppermint tea, dreading the thought of trying anything that might give me cramps and send me to the bathroom in the middle of class or social situations.
My worried parents demanded that I see another doctor. I did. I saw two, in fact, and both of them suggested the source of my weight loss and anxiety about eating were only related to stress. One prescribed an anti-spasmodic medication that she thought would keep my stomach from feeling fine one minute to cramping the next. The medicine didn’t really help and when I mentioned this to the other doctor, he chastised me for being one of the many young people who just want a “quick fix”.

I avoided the doctors from then on. I stayed away from the foods that I knew were bad for me and tried to eat as many “safe foods” as I could. I finished grad school and started work. I came to accept certain times of the year as times when my IBS would flare up, but I never stopped trying different supplements, yoga, journaling, and meditation techniques to keep my symptoms from taking over my life. I felt like I could manage well enough.
This summer I began experiencing terrible symptoms once again, worse than before. On top of diarrhea several times a day, I had a fever that would come and go. I’d feel exhausted by simple tasks and didn’t want to do anything but stay in bed. As much as I didn’t want to, I turned to a new doctor, who ordered a routine CT scan that I was lucky enough to be able to have done the next day. But because it was “routine,” I couldn’t expect results for a few more days. My body couldn’t wait. That night I was up with the worst pain of my life. I was passing nothing but bile and mucus, and could hardly sit up. It felt like I had a bowling ball pressing against my rib cage, and my belly was swollen. I went to an urgent care facility where the doctor there was able to expedite the report on my CT scan. She was surprised to learn that no one had ever told me that I clearly had Inflammatory Bowel Disease, not just IBS. While the symptoms are pretty similar, IBD is much more serious. Every person experiences it differently, but the damaging effects of IBD are far-reaching and can impact every aspect of a person’s life.
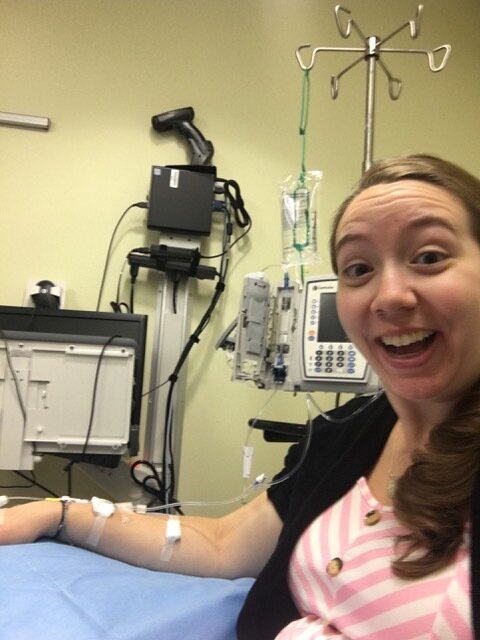
Now that I had this new label, I was frustrated that it had taken so long, but also glad that I now had an answer. I met with a new gastroenterologist who was kind and supportive. He formally diagnosed me with severe Crohn’s Disease and immediately started me on steroids to lower my inflammation. He also started me on Infliximab, a biologic medication that I would get infused into my body every few weeks.
Hopefully this would treat the fistula that had developed in my small intestine and prevent the need for surgery anytime soon. Things seemed promising. So here we are. I’m still on the steroids, but my body has started rejecting Infliximab. I had to quit my job as a school teacher. I’ve had another hospital stay, and have now started Humira, a different biologic that may or may not help. All I can do now is watch, wait, and hope. I track my diet and any effect it has on my symptoms, and wait to see whether the new medication changes the way I feel. I hope that somewhere in this struggle I can start to feel like myself, the bright and shiny person I used to be.
Through all the hits and misses with doctors and treatment, through all the highs and lows of symptoms and relief, I’ve come to learn a lot about myself. I’ve come to rely on humor to get me through the days of feeling powerless and useless. I’ve come to rely on the genuine compassion from my friends and loved ones. I’ve come to rely on my own ability to empathize with others who are suffering from similar diseases and all their effects. Despite the struggles and the unknown challenges ahead of me, I can honestly say that this process has turned me into something of an optimist. And for that, I’m truly grateful.
Stephanie Maguire is a fun-loving goofball who lives in Virginia with her fiancé. She is a former elementary school teacher and current yoga teacher whose hobbies include watching movies and going outside.
