IBD | Information
Image of the author holding a Humira pen.
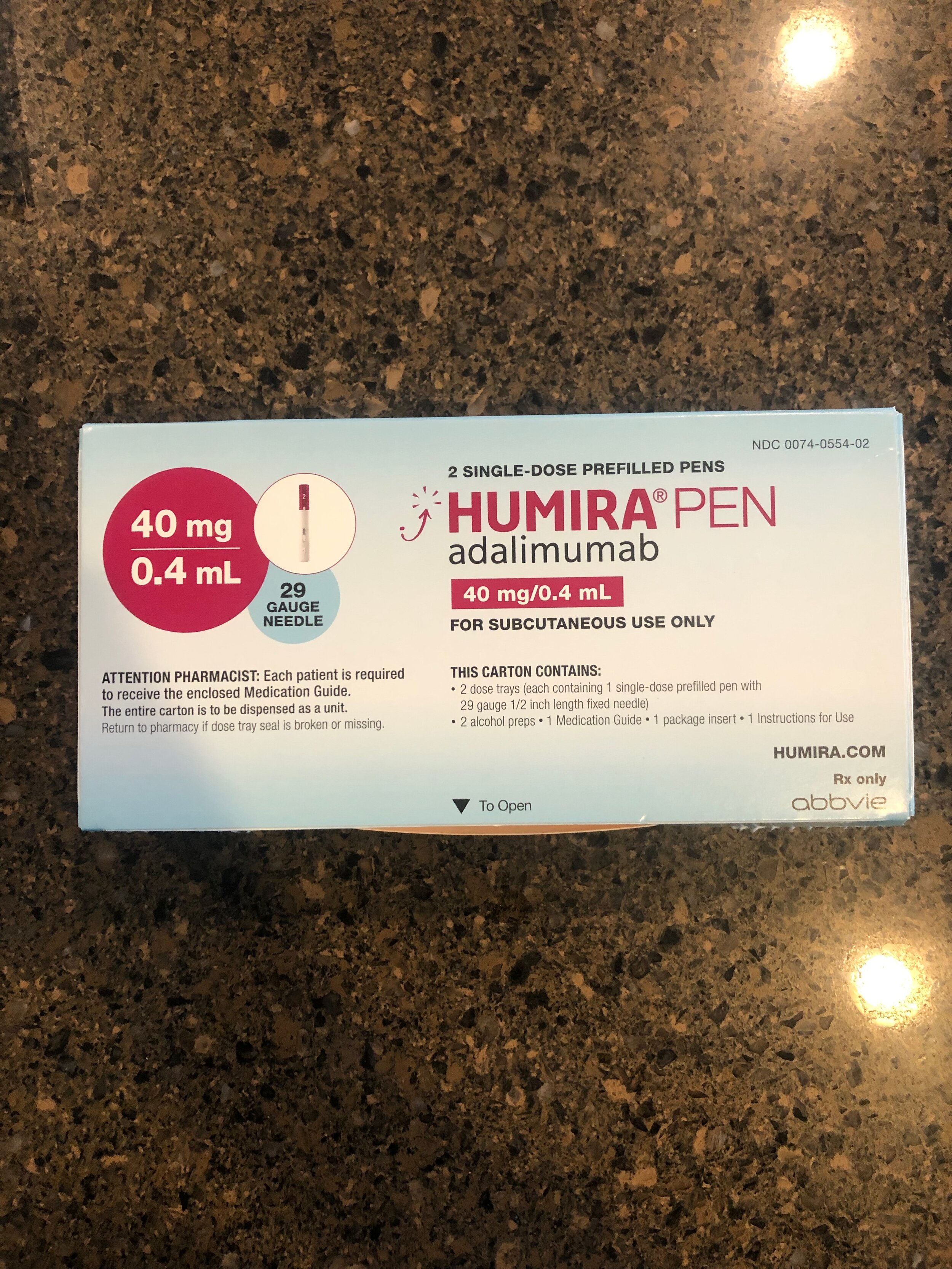
When I was initially diagnosed with Crohn’s disease, my physician immediately recommended Humira (part of me feels as though I sound like a drug ad campaign right now, but stick with me!). Upon starting treatment, my main concerns were over the feasibility of injecting myself, staying on top of treatments, and reaching remission. Once my first injection arrived, these concerns changed – I was shocked by the cost of IBD treatment. Fortunately, my insurance fully covers Humira after reaching my deductible but seeing a price tag of several thousand dollars is intimidating.
At full retail cost, the average cash payment for a single month of Humira pens is about $9,351.38. Even more alarming, this price has been steadily increasing despite no significant formulary alterations since making the switch to citrate-free. Looking at just this year, the cost of a monthly supply of Humira pens in January was about $8,618.69 meaning the cost has increased by approximately $732.69 in a five-month timeframe. For reference, Humira generally has to be taken every two weeks, making the yearly cost of treatment around $112,216.56.
Now, companies will respond to this by telling patients to just utilize their insurance to cover the cost; however, the truth is not every individual can afford to pay for insurance each month despite desperately needing treatment. Even with insurance, individuals may not be able to afford costly deductibles and medication co-pays. They will then tell you to utilize a savers card to bring the cost down to a more reasonable price. When systems like this work, it is great for ensuring patients get their medication. With that being said, these cards can still get rejected, ultimately forcing a patient to forgo treatment. If you are uninsured, the recommendation will be to use a drug assistance program. Just as with pharmaceutical saving cards, these programs can be hit or miss – sometimes an individual will get covered and other times not.
Ultimately, this means certain individuals will be stuck with a significant bill for their medication. And in many cases, this leads to ceasing a desperately needed treatment plan. Even for patients lucky enough to get a savers card or drug assistance program, it can take up to several months to verify eligibility. This can lead to months of delayed treatment if a patient does not have access to physician samples.
This alone may sound frightening – but wait there’s even more! Imagining that biologics are the only therapeutic option an IBD patient will utilize is unfortunately wishful thinking. Patients may require treatments for comorbidities associated with IBD such as infusions for anemia or vitamin deficiencies and therapy or medication options for mental health complications. In order to manage symptoms, patients may also utilize other anti-inflammatory pharmaceuticals or painkillers. Patients will need to undergo different testing throughout their lifetime in order to ensure management of their condition such as colonoscopies, capsule endoscopies, and frequent lab work. During times of uncontrolled disease, surgery or a feeding tube may be necessary meaning associated hospital fees as well. Patients with ostomies will also need to purchase an array of supplies for hygienic maintenance of their stoma/pouch. Let’s not forget the time and money lost from missing work for appointments, surgeries, or treatment recovery. For individuals struggling with IBD, work may not even be an option due to condition severity also meaning employer-covered insurance could be lost.
Healthcare costs for IBD patients are more than three times that of non-IBD patients with average out-of-pocket costs twice as much in patients with IBD when compared to those without. Additionally, IBD patients are estimated to have a three times higher work-related loss in wages than non-IBD patients.
Insurance coverage or not, IBD treatment can get expensive and the battle to get or maintain coverage can be incredibly stressful. Being only 23 and still fortunate to be under my parent’s insurance, there have been multiple occasions when I have worried about how I will afford my treatment once I am off my parent’s insurance. Will I have a job with great benefits to pay for my Humira and associated therapeutics? Will I be able to afford a commercial payer insurance that supports my medical needs? With all the costs discussed above, I sure hope so.
The ultimate point of all this is that the affordability of IBD treatment can be excessively unrealistic and that patients should not have to forgo needed therapeutics due to cost. No one asks to be diagnosed with IBD or to have the associated financial burden of their condition. With that being said, I also understand no one asks to be put into a position of advocacy but having IBD does just that. As individuals, we have to unite as a community in advocating for realistic treatment costs regardless of whether we ourselves can afford treatment or not.
Additional Reading
Crohn’s and Colitis Foundation. “The Cost of Inflammatory Bowel Disease” (20 August 2019); accessed 18 June 2021 https://www.crohnscolitisfoundation.org/cost-inflammatory-bowel-disease
