IBD | Information | Ostomy
It’s officially summer! In addition to sun, swimming, and bonfires, summer means another huge thing for us IBD girls and ostomates- increased risk of dehydration. To talk about this issue with friends and experts in our community, we hosted a Twitter Chat to talk all things hydration! Joined by registered GI clinic dietician Mandi Stayner (@mandistaynerRD) of Froedtert Hospital in Milwaukee, ostomate and patient advocate Alison Rothbaum (@empoweringpts9) of Empowering Patients, LLC and our friends at DripDrop (@drinkdripdrop), we were able to have a great chat! In case you missed it, here’s a brief recap of what was discussed:
1. IBDers become dehydrated more easily because inflammation and/or surgery can make it difficult to absorb water and nutrients. Absorption is a particular concern depending on the location of your disease and remaining anatomy after surgery- the colon is primarily responsible for absorbing fluids. Nausea, vomiting, and diarrhea are all complicating factors. Additionally, some medications can make controlling your body’s thermostat more difficult and increase fluid/electrolyte loss via sweat.
2. Outdoor activities during the summer months can be especially brutal when it comes to fluid loss. Breaks in routine due to outdoor adventures and vacations can also make it difficult to remember to hydrate. Placing cooling towels around the neck and setting alarms for drink breaks are two things that can help to retain and replenish fluid when busy outdoors.
3. Your body will let you know when you’re dehydrated! While thirst is the most obvious reminder, headaches, dizziness, decreased urine output, dark urine, fatigue, dry skin, increased heart rate, low blood pressure and muscle cramps are all signs of depleted fluids and electrolytes. Take care to pay attention and not ignore these symptoms if they appear.
4. There are some gadgets on the market that can help remind you to hydrate and alert you when things are going downhill. These include the Ulla Smart Hydration Reminder for water bottles and wearable technology like the Apple Watch or Fitbit than can alert you of rising heart rate. Utilizing technology for this purpose can be as simple as setting regular alarms on your phone.
5. With an ostomy, especially an ileostomy, it’s extremely easy to get dehydrated since there’s no colon to reabsorb liquids. Measuring your output can be very helpful to keep you on top of hydration. Consistency is also important. The more watery your output is, the more fluid you’re losing. @mandistayner stated that she and her team aim to keep their patients at under 1200 mL of ostomy output daily.
6. Certain foods, depending on each person, can cause increased ostomy output, which can easily lead to a need for increased fluid intake. This often includes foods that have high fat, sugar, and/or fiber content and sugar alcohols.
7. Options that may help to decrease ostomy output include banana, oatmeal, white rice, applesauce, white bread, crackers, and marshmallows. Soluble fiber supplements like pectin (the same stuff you use for making jelly/jam), Citrucel, Metamucil, and Banantrol may also help to slow things down.
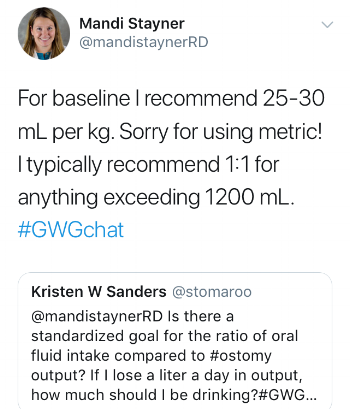
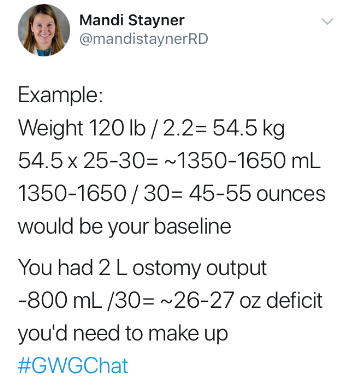
8. @mandistayner had some great recommendations for calculating appropriate fluid replacement volumes based on your ostomy output:
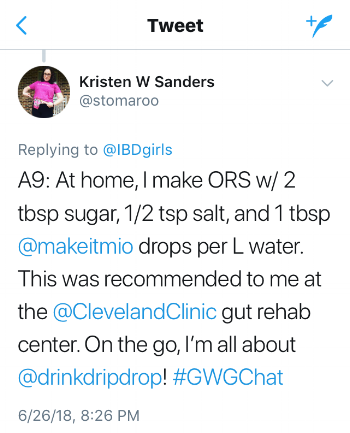
9. Oral Rehydration Solutions (ORS) are key to maintaining hydration status when you have increased loss of fluid via the GI tract. Increased GI losses also equals the loss of electrolytes (like sodium, potassium, chloride, and magnesium). ORS contain these salts in addition to some sugar (glucose) to that helps to pull them across the cell barrier of the intestinal mucosa to be absorbed into the bloodstream. Recommended ORS products include DripDrop and Nuun.
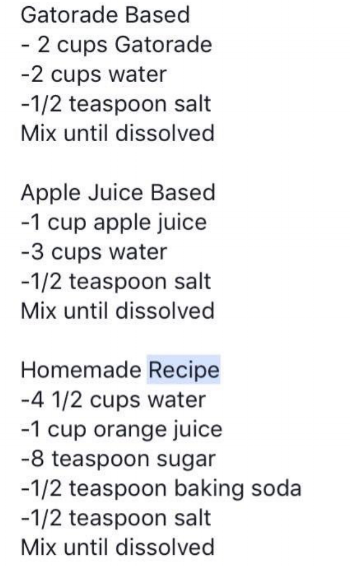
10. Several individuals shared their recipes for making ORS at home: